Lawrence Tanenbaum is a big believer in AI, as a tool to create better images, offer a more comprehensive view of a patient and more effectively handle imaging’s increasing volume and complexity. Bigger yet, AI is the impetus to change the way radiology and medicine are practiced across the care spectrum.
Taking care of outpatients, lots of them, is the focus for this 30-year radiology veteran who is the vice president and medical director for the East Region of the largest provider of free-standing, fixed-site outpatient imaging services in the U.S., RadNet. Their 500-plus radiologists at 298 owned or operated outpatient imaging centers read more than 7 million scans a year—so Tanenbaum sees great value in facilitating those reads and strengthening the fabric of radiology.
Staff better, utilize assets better, scan better, triage better, see better, read better, predict better, report better, bill better. That is Tanenbaum’s vision of how AI will mediate human performance and enhance people’s ability to perform tasks and change the way they do so. “The explosion of smart algorithms is going to increase both the value of the radiologist and imaging,” he says. “Imaging needs AI, and we need to be gearing up now. It’s all happening very quickly.”
A radiologist with a ruler is not delivering maximum value, he jokes. We need to leverage advanced technology and greater knowledge to deliver the critical information which sets the next step in the diagnostic or treatment pathway.
We are beginning to reap the benefits of AI, with radiology one of the hottest areas of AI in terms of available options, Tanenbaum notes. “In just a few years, it’ll be almost a given that we won’t address an imaging study without a computer taking a look at it first. It’ll triage, highlight and pre-process and we as radiologists will connect the dots.”
He sees radiologists having more time with patients or to contemplate the information they’ve never had at their fingertips like genomics and patient history along with AI-generated information. “We’ll escape the information vacuum, delivering much greater value along with greater job satisfaction. This will enhance what we can produce.”
Behind the scenes, Tanenbaum is excited about AI algorithms balancing workloads (burning out burnout!) and triaging cases that need urgent attention or immediately notifying radiologists of urgent findings such as a stroke or pneumothorax. “I see value in simplifying analysis of cases that have multiple time points by assisting in the longitudinal analysis of interval change. Or in doing screening examinations, which should increase in volume, by facilitating the identification of normals as well as detecting early signs of malignancies too subtle for human perception but detectable by trained algorithms.”
Gains will come too in operational and financial advantages efficiencies. Think better asset and staff utilization and effective billing by determining which claims will be rejected. Algorithms will determine the best deployment of assets, such as where a ultrasound system should be located, and offer recommendations on the likelihood of a patient’s readmission to a hospital or developing complications or certain diseases.
Revolutionary will be AI’s ability to change the amount of scan time necessary to create an MR image, for example, or the amount of contrast for contrast-enhanced imaging. “We’re going to see the next generation of noise reduction in CT that’s going to be more clever and allow even greater dose reduction. We’re going to see smarter tools like reconstructions that will recognize motion.” He also points to the ability to diagnose lung cancer multiple visits before a radiologist can detect it visually or detect fractures, hemorrhage, stroke or pneumonia and bring those cases to the top of the worklist.
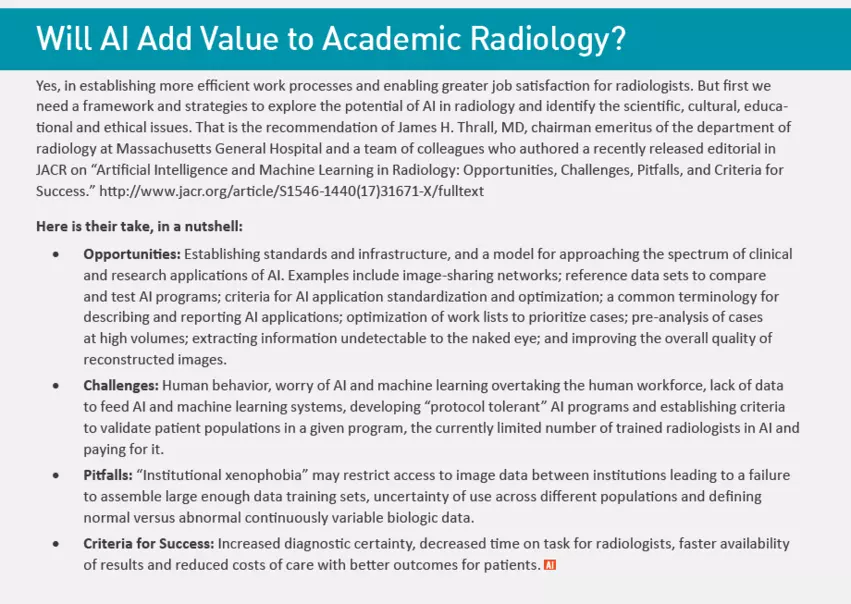
But there are concerns too. “One of the biggest challenges to the growth of imaging AI is organizations adopting new strategies restricting data access,” he says. “Typical privacy issues as well as concern over lost value [in data] may serve as a substantial retardant to advancement.”
It is said that “radiologists will not be replaced by AI, but radiologists who don’t use machine learning techniques will be replaced by those who do.” In reality, Tanenbaum expects AI capabilities to ultimately integrate seamlessly into the radiologist’s user interface and thus be unavoidable as we move forward.
His battle cry is to get ahead of the curve and stay on top of developments. “We need to strive to be early adopters so that we can rapidly integrate these new tools in our clinical practice settings.”
That means having progressive infrastructure to support real-time medicine. “We have bottlenecks now that could very well retard our progress,” he notes. “There is a good potential to share large volumes of data via the cloud. We’re still suffering with bandwidth limitations. We need to seek out solutions to coax data out of locked silos and moving seamlessly.”
Finding the right solutions in and adopting the right technologies to allow AI to succeed requires “a healthy dose of intellectual curiosity, an early adopter mentality and imagination as to what these tools can do,” Tanenbaum says. “And a big healthy dose of caution and skepticism too. That’s how we change care.”